Mastering Phlebotomy Testing: Essential Tips for Accurate Blood draws and Lab Results
Phlebotomy testing sits at the crossroads of patient care and laboratory science.A successful blood draw is more than just inserting a needle-it requires precise technique, strict adherence to safety, and meticulous handling of specimens to ensure accurate lab results. In this thorough guide, you’ll discover proven strategies for mastering phlebotomy testing, from patient preparation to post-collection handling, with practical tips you can apply in clinical settings today.
What is Phlebotomy and Why It Matters
Phlebotomy is the process of obtaining blood samples for laboratory analysis. The quality of the sample and the reliability of the resulting lab data depend largely on the pre-analytical phase-everything that happens before the specimen reaches the analyzer. Factors such as patient preparation, method of venipuncture, tube selection, labeling accuracy, and timely transport all influence test accuracy, turnaround times, and patient safety.
Understanding the role of phlebotomy within the broader clinical lab workflow helps clinicians and technicians recognize how small decisions impact diagnostic decisions, treatment plans, and patient outcomes. Mastery of phlebotomy testing is therefore an essential skill for nurses, phlebotomists, lab assistants, and all healthcare professionals involved in specimen collection and handling.
Essential Tips for Accurate Blood Draws
1) Thorough Patient Preparation
- Verify patient identity using at least two identifiers (full name and date of birth) before drawing.
- review the order for fasting requirements, recent medications, and known allergies or bleeding disorders.
- Explain the procedure in plain language to reduce anxiety and improve cooperation.
- Ask about venous access history (e.g., challenging veins, prior phlebotomy challenges) to tailor technique.
2) Site Selection and Aseptic Technique
- Prefer antecubital fossa veins when feasible; avoid areas with scarring, edema, infection, or fistulas.
- Apply the tourniquet 3-4 inches above the venipuncture site and limit its use to under 60 seconds to prevent hemoconcentration.
- Cleanse the site with an appropriate antiseptic (e.g., alcohol impregnated swabs in concentric circles) and allow it to air dry completely before needle insertion.
- Anchor the vein with the non-dominant hand to stabilize the vessel and reduce movement during puncture.
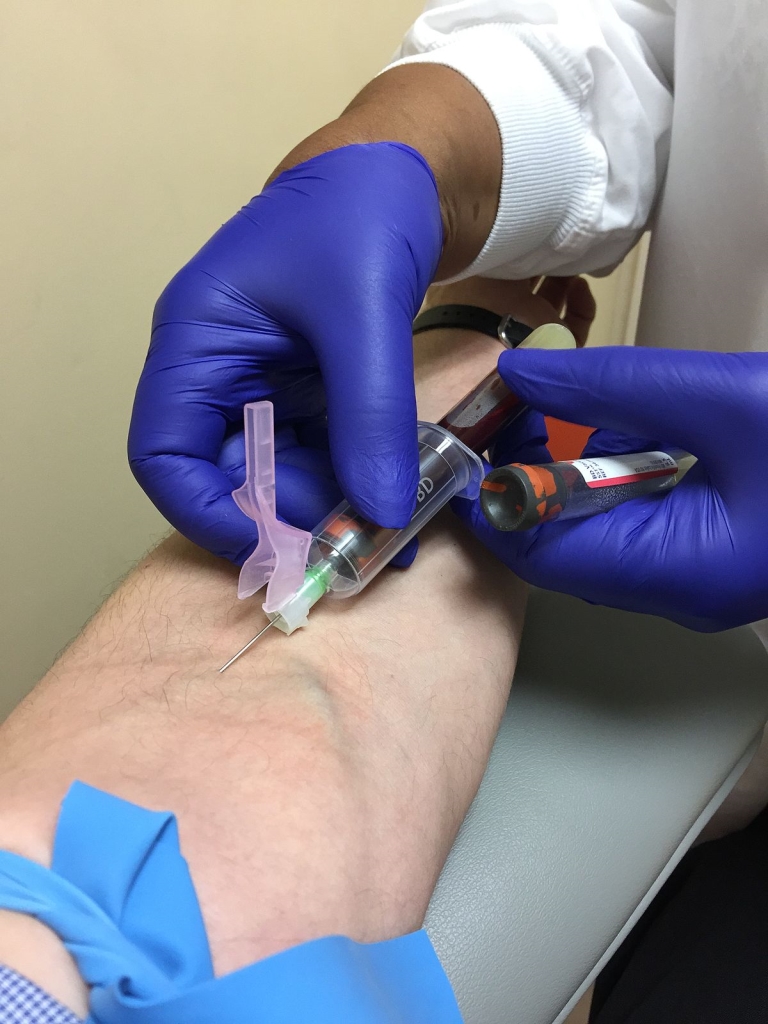
3) Venipuncture Technique and Equipment
- Choose the correct needle gauge (commonly 21-23 gauge for adults) and use the smallest gauge that suits vein size to minimize trauma.
- Stabilize the needle with a steady hand, insert at a shallow angle (approximately 15-30 degrees), and advance smoothly into the vein.
- Be mindful of patient pain and adjust technique if the patient experiences unexpected resistance or movement.
- Attach vacuum collection tubes in sequence, ensuring proper tube placement and orientation for each additive.
4) Tourniquet Use and Patient Comfort
- Limit tourniquet time to under a minute; remove as soon as blood flow is established.
- Consider option strategies for difficult veins, such as warming the hand or using smaller gauges, while maintaining patient comfort and safety.
- Provide clear instructions on post-draw care to reduce bruising and hematoma formation.
5) Order of Draw and tubes
- Follow a standard order of draw to minimize cross-contamination of additives.A common sequence is: blood culture tubes (when ordered), light blue (citrate), serum tubes (red or gold SST), green (heparin), lavender (EDTA), grey (fluoride/oxalate). Always comply with your institution’s protocol.
- Mix tubes gently by inverting the specified number of times per additive to ensure proper anticoagulation or clot activation.
6) Labeling and Documentation
- Label tubes at the patient’s bedside, not after leaving the patient room, to ensure accuracy.
- Include essential identifiers: patient name, date of birth, unique medical record number, date/time of draw, and initials of the collector.
- Double-check labels against the patient’s wristband or chart to prevent mislabeling errors.
7) Handling and Transport
- Invert tubes gently to mix additives as required; avoid vigorous shaking that can cause hemolysis for certain tests.
- Maintain appropriate temperature ranges during transport (e.g., some chemistry tests require room temperature, others refrigeration).
- Document any deviations (delays, temperature excursions, traumatic draws) and communicate with the laboratory promptly.
8) Minimizing Pre-Analytical Errors
- Avoid drawing from an IV line unless policy allows and appropriate flushing is performed to prevent sample dilution with IV fluids.
- Address difficult venipuncture with alternative sites or devices (e.g., butterfly needle, smaller gauge, or ultrasound-guided techniques in certain cases), while documenting the approach.
- Ensure proper sample volume for pediatric or elderly patients to prevent the need for redraws due to insufficient volume.
Common Pre-Analytical Errors and How to Prevent Them
Even a technically sound venipuncture can fail to yield reliable results if pre-analytical errors creep in. Here are the most common issues and practical prevention tips:
- Hemolysis: occurs from excessive tourniquet time, rough handling, or using a small needle. Prevention: use appropriate needle size, gentle technique, and prompt handling.
- Incorrect tube type or missing additives: ensure the correct tube is collected for each test and confirm additives before drawing. Prevention: review the test panel and fill order before venipuncture.
- Clotting of plasma or serum: mix tubes as instructed and avoid using clotted samples for tests requiring whole blood or plasma. Prevention: invert the tubes the recommended number of times after collection.
- Contamination from IV lines: draw from a discontinuous venous access only when guidelines permit; flush lines as appropriate. Prevention: document line status and consider alternate sites.
- Mislabeling: mislabeled samples lead to diagnostic errors. Prevention: bedside labeling, two identifiers, and cross-checks against the patient’s chart.
- Delayed transport: prolonged time before reaching the lab can degrade some analytes. Prevention: schedule prompt transport and use proper packaging.
- Insufficient sample volume: repeatedly drawing increases patient burden. Prevention: plan collection according to the test menu and consider pediatric-adapted strategies.
Tip: Establish a standardized checklist for every draw. Checklists reduce errors by ensuring consistency across shifts and staff levels.
Quality Control in Phlebotomy
Quality control in phlebotomy goes beyond the collection bench.It encompasses training, equipment maintenance, procedure standardization, and continuous enhancement. Key elements include:
- Regular training and competency assessments for phlebotomy staff.
- Documentation of incidents, deviations, and near-misses with corrective actions.
- Maintenance of a clean, organized workspace with readily available supplies to minimize delays.
- Calibration and verification of equipment (needles, holders, tourniquets, vacuum tubes) and proper storage of additives.
- Quality indicators such as redraw rates, specimen labeling accuracy, hemolyzed samples, and transport times tracked over time.
Quality control also means fostering a culture that prioritizes patient safety, patient-centered care, and teamwork between phlebotomy staff and laboratory personnel.
Practical Tips and Best Practices
- Keep patient comfort in mind: explain every step, ask for permission before palpating, and monitor for signs of distress.
- Stay organized: prepare all tubes in the correct order before approaching the patient to avoid delays.
- adopt a patient-friendly approach for difficult draws, including warming the extremity, selecting alternate sites, or using ultrasound guidance when appropriate and trained.
- Protect patient privacy and data integrity; label and document discreetly and securely.
- Document special considerations (diabetes, anticoagulation, anemia) that may impact drawing technique or tube choice.
Pro tip: when in doubt about a test panel, coordinate with the lab to confirm the required tube type and volume. Clear dialog reduces needless repeats and improves turnaround times.
Case Studies and First-Hand Experience
Real-world anecdotes highlight the importance of good technique and meticulous handling:
case Study 1: Difficult Venous Access in an Elderly Patient
A 78-year-old patient with fragile veins presented for routine metabolic testing. the phlebotomist used a smaller gauge butterfly needle, warmed the hand, and anchored the vein. By selecting the most accessible vein and avoiding multiple punctures, the team obtained sufficient volume with minimal discomfort. The lab received properly labeled samples with no hemolysis or contamination, resulting in a smooth workflow and timely results.
Case Study 2: Preventing Hemolysis in a Busy Emergency Department
During peak hours, a high volume of draws led to occasional hemolyzed samples. A targeted intervention included reinforcing gentle inversion, avoiding excessive shaking, and standardizing the draw order. After implementation, the hemolyzed rate dropped, and test validity improved, notably for potassium and AST/ALT panels.
Case study 3: Accurate Labeling to Avoid Mix-Ups
A small outpatient clinic implemented bedside label printers and double-check procedures for patient identifiers. The result was a dramatic reduction in mislabeling events, fewer rejected specimens, and faster patient discharge with reliable results.
Benefits of Mastering Phlebotomy
- Improved diagnostic accuracy and faster turnarounds for clinicians and patients.
- Enhanced patient safety with fewer complications such as hematoma, infection, or labeling errors.
- Reduced need for repeat draws, saving time and reducing patient distress.
- Better data integrity for laboratory data systems and clinical decision-making.
- Greater professional confidence among phlebotomy staff thru structured training and ongoing quality improvement.
Quick reference: Common Tests, Tube Types, and Draw Order
Use this concise guide to support daily practice. Always follow your institution’s standard operating procedures, but this table offers a pragmatic overview.
| Test Type / Purpose | Recommended Tube Type | Common Additive | Notes |
|---|---|---|---|
| CBC (Complete Blood Count) | Purple/Lavender top | EDTA | Glass or plastic; ensure proper mixing by gentle inversion |
| BMP/CMP (Basic/Fast Metabolic Panel) | Red or Gold SST | None (red) or serum separator (SST) | Serum required; invert to mix |
| Coagulation Studies (PT/INR, PTT) | Blue top | Citrate | Fill to fill volume for accurate ratio |
| Blood Cultures | Special culture bottles (aerobic/anaerobic) | Growth media | Draw prior to antibiotics when possible |
| Glucose (Fasting/Random) | Grey top | Fluoride/oxalate | Timely processing for accurate glucose |
Note: The exact order of draw may vary by protocol; consult your lab’s standard operating procedures for precise guidelines.
Conclusion
Mastering phlebotomy testing is a blend of science, safety, and patient-centered care. By focusing on thorough patient preparation,precise venipuncture technique,correct tube handling,accurate labeling,and timely specimen transport,healthcare teams can dramatically improve the reliability and speed of lab results. Regular training, adherence to standardized procedures, and a culture of continuous improvement are the cornerstones of quality phlebotomy practice. Whether you are a seasoned technologist or new to the field, the tips and best practices outlined in this guide can help you deliver safer, more accurate blood draws and contribute to better patient outcomes.
If you’re looking to elevate your phlebotomy skills, consider implementing a bedside labeling protocol, a draw-order checklist, and routine quality audits. Small, consistent changes compound into meaningful improvements that benefit patients and the entire clinical laboratory ecosystem.
Ready to improve your practice today? Start with a quick checklist, train your team on the key steps, and commit to continuous improvement in every blood draw.